Cardiology was technically our first 3 week module, and it was a little weird to have two weekends to study instead of the typical one. I honestly think that allowed me and my classmates to be more relaxed during the first week of study... which is a good and bad thing! I felt like I didn't study as much as I should have at the beginning, but I got enough studying in the last 2 weeks to last me a while... Plus I feel that I had a major interest in cardiology and cardiothoracic surgery so it made it easier to retain the info.
One skill we have been working on since we started the program is ECG interpretation, and I know SO much more than I did when I started... but let me tell you, it is not easy to pick up. It is a skill that gets mastered over time, and as one of our professors says: "you have to practice this skill over and over again in order to become and stay proficient". I really enjoy it, however, it will take me lots more practice until I feel comfortable interpreting them.
Here is a bit-o-knowledge from Cardiology:
Auscultation (listening with the stethoscope) for cardiac murmurs and bruits is a skill that takes a lot of experience and practice. Of course its not always easy to hear pathology on fellow classmates who are all normal...
Bruits (pronounced brew-ees) is a sound produced from non-laminar flow (disruption in normal blood flow). This can be due to plaque or a clot. Below is a typical presentation that can cause a bruit.
 |
| Plaque that can cause a Carotid Artery bruit |
A typical treatment for a carotid artery plaque (if it is severe enough, and a risk for emboli) is a carotid endarterectomy. As the photo shows, just cut the artery open, take out the plaque, and sew it back up. Some times a shunt will be placed around the plaque in the artery to continue blood flow while the plaque is removed. Clamping off the carotid for surgery can only be done for a short amount of time due to its effect on brain blood flow (that's kind of important!)
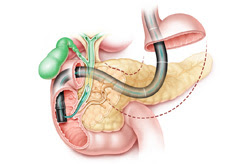
GI Module
I never thought I would have such an "intimate" relationship with the colon and feces as I did during GI. I feel so much more comfortable with poop, bowel sounds, asking patients about their bowel habits, blood, hemorroides, and of course prolapsed rectums!
One of our guest lecturers (a colorectal surgen) spoke about how "you can learn a lot about a patient by sticking your finger up their butt"... the whole class laughed a lot during that lecture. It was a really interesting module because this is something that will be addressed a LOT in practice. A lot of patients will present with GI upset from drugs they take, or constipation. And because everyone needs to eat to live... i'd say there is a lot of things that can go wrong. Also there is a lot of people who like to do some weird things and get "items" stuck in their rectum, so they present to the ER for help. (Yep, we got to see pictures of that too!)
I also had the opportunity to do some dissection in the cadaver lab for the upcoming anatomy test involving the GI tract. It was really fun, and time really went by fast when I was dissecting. I spent a solid 5 hours in the lab dissecting and I hardly noticed it. I love working with my hands and I enjoy learning about the body hands on. It helped me to understand the anatomy so much better.
For those wanting to attend Pacific... ask about the opportunity to do some dissections... you don't have to do them, but if you don't, you'll miss out on an amazing opportunity. The program doesn't set aside "scheduled time" for you to dissect, but there is time available during scheduled lab time where dissections can be performed. Plus you get to help dissect out what is going to be on the test, so you get a much better understanding of where the structures are on the cadavers.